By Anthony V. DeIorio Jr., MD, FACS
 In discussing colon health, there are two key factors to consider. First, to achieve a healthy colon, one must regulate diet and supplements to normalize bowel movements. Crucial to that is the incorporation of fiber within the diet either through the foods eaten or a fiber supplement. I am often asked how much fiber supplement should be taken. The amount of supplement should be determined by the amount of fiber in the diet. That is, a patient who takes in a fair amount of fiber within the diet in the way of fruits and vegetables probably doesn’t need supplementation. A patient who takes in only a moderate amount of fiber within the diet may need only a small supplementation. And, one with very little fiber in the diet may need full supplementation. In addition and equally important, is the consumption of water with any variety of fiber. Fiber serves to bulk the stool but water must be incorporated to soften it. Daily intake of water should be approximately 6-8 eight ounce glasses. The adequacy of the amount of fiber and fluid can be judged by the consistency of stool being solid but soft. Also, a patient can consider the use of probiotics particularly if he/she had recently been on antibiotics recently.
In discussing colon health, there are two key factors to consider. First, to achieve a healthy colon, one must regulate diet and supplements to normalize bowel movements. Crucial to that is the incorporation of fiber within the diet either through the foods eaten or a fiber supplement. I am often asked how much fiber supplement should be taken. The amount of supplement should be determined by the amount of fiber in the diet. That is, a patient who takes in a fair amount of fiber within the diet in the way of fruits and vegetables probably doesn’t need supplementation. A patient who takes in only a moderate amount of fiber within the diet may need only a small supplementation. And, one with very little fiber in the diet may need full supplementation. In addition and equally important, is the consumption of water with any variety of fiber. Fiber serves to bulk the stool but water must be incorporated to soften it. Daily intake of water should be approximately 6-8 eight ounce glasses. The adequacy of the amount of fiber and fluid can be judged by the consistency of stool being solid but soft. Also, a patient can consider the use of probiotics particularly if he/she had recently been on antibiotics recently.
Second, regular maintenance evaluations of the colon should be undertaken in the way of colonoscopy. In general, the current recommendations from the American Cancer Society include commencing colonoscopy at age 50, earlier if there is a family history or genetic predisposition to colon cancer. Follow up colonoscopies are determined by the findings. If there are no findings on the initial scope, subsequent colonoscopy can be performed in 5-10 years. If polyps are identified and removed, follow-up colonoscopy should be considered in 3-5 years.
So what if the colonoscopy is abnormal?
Common treatable findings can include everything from colitis to inflammatory bowel disease to diverticular disease to hemorrhoids to polyps to cancers.
Colitis is simply an inflammation of the colon. It can be infectious or ischemic in origin. Infectious colitis can arise from viral or bacterial infections. Viral colitis is treated symptomatically with medications until symptoms resolve. Bacterial colitis is treated with antibiotics as well as symptomatically with medications until symptoms resolve as well. Ischemic colitis can resolve on its own or may need surgery to remove the involved portion of colon.
Inflammatory bowel disease exists in two varieties, Crohn’s disease and ulcerative colitis. Crohn’s disease is an autoimmune inflammatory process which can affect any part of the GI tract. It is usually a transmural inflammation, that is it affects the whole wall of the intestine. It presents most often with abdominal pain and diarrhea, usually associated with some bleeding. It is diagnosed by endoscopy and biopsy. Treatment consists of medications that counteract the inflammatory process causing the disease, such as steroids. Surgery is only done for intractable symptoms that cannot be resolved medically. Cancer is not generally associated with this disease process. Ulcerative colitis attacks only the colon and generally only affects the inner layer of the colon called the mucosa. It also can present with abdominal pain, diarrhea, and bleeding. Colonoscopy with biopsy can diagnose this process. Complete removal of the colon and rectum by surgery is curative. If surgery is not performed, the risk of colon cancer becomes significant if the disease has been in place for greater than 10 years.
Diverticular disease involves outpouchings of the colon wall that occur at natural weak points such as where blood vessels penetrate the wall. These commonly occur in the sigmoid colon on the left lower part but can occur elsewhere. Often, they are asymptomatic and require no treatment. They can become inflamed producing diverticulitis, which is usually treated with antibiotics unless it becomes a complex infection. Complex infections include perforating the colon, abscesses, and strictures. These complex entities often require surgery to repair the process. Diverticula can cause bleeding as well. This, too, can be managed medically in many circumstances, but if intractable, would warrant surgery.
Hemorrhoids are a common finding on endoscopy. Many are asymptomatic and require no treatment. Inflammation of the hemorrhoids is generally treated medically. Surgery is reserved for those hemorrhoids that are resistant to medical treatment or repetitively bleed.
Colon polyps are also common to find on colonoscopy. Most of these can be removed with the scope. There are a variety of colon polyps that have differences as to whether or not they are precursors to cancer and the degree of risk of whether it would become a cancer. Some polyps are identified that are too flat or too large to be removed endoscopically. These polyps would warrant surgery to remove that segment of the colon.
Cancers of the colon are also identified on colonoscopy and diagnosed by biopsy through the scope. These are treated by surgical removal of the involved segment of colon together with the lymph nodes draining that segment. A cancer stage is determined by the findings on the surgical specimen read by the pathologist. More advanced stages are treated after surgery with chemotherapy. Now certain biochemical tests are also run on these cancers to determine if the cancer will be aggressive, warranting chemotherapy even in earlier stages. Cancers of the rectum are generally treated before surgery with radiation. Subsequently, surgery removes the segment of rectum and involved. Chemotherapy may be employed after surgery here as well.
Surgeries to perform colon resections are done and a variety of ways. Open abdominal surgery through an incision is the oldest and one of the more common ways of accomplishing the task. Some conditions are amenable to laparoscopic surgery. In general, laparoscopic surgery on the colon provides for an identical result in the way of cure of the disease process; however, it may allow for a slightly quicker recovery. Open colon resection patients generally are in the hospital 7-10 days with full recovery in 4-6 weeks. In contrast, laparoscopic colon resections usually leave the hospital in 4-5 days with full recovery in 3-4 weeks. Additionally, now many surgeons are learning to perform some colon resections robotically. The biggest purported advantage of this technique is in even more rapid recovery of 3 days in the hospital and approximately 3-4 weeks for full recovery.
I do hope the above overview of colon health and common disease processes was helpful to those of you who read it. Certainly, any questions about the above can be discussed with either one’s primary medical doctor or at a consultation with the general surgeon.
Munroe Regional Medical Center
Ocala Surgical Associates
1541 SW 1st Avenue
Ocala, FL
(352) 622-8152
Check Also
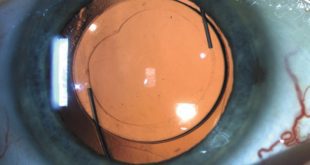
CUSTOMIZABLE LIGHT ADJUSTABLE LENS A GAMECHANGER FOR CATARACTS PATIENTS
All Americans have some degree of cataract change by the age of 75. As the …
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages