With the implementation of ICD-10 upon us, is your office staff confident and ready for the transition?
A lack of readiness and compliance could result in widespread disruptions of payments to your practice when claims bearing ICD-9 codes are rejected.
As with ICD-9, ICD-10 is based on the International Classification of Diseases, published by the World Health Organization, which designates unique codes to identify health conditions and reasons for medical services. It offers more than 68,000 diagnostic codes, compared to 13,000 in ICD-9-CM, and introduces alphanumeric category classifications for the first time. As such, ICD-10 is much more proficient at describing current conditions and healthcare practices. These new codes posses the flexibility to expand in order to accommodate advancements in clinical medicine.
What does the change represent for your office?
As providers, you are ultimately the source of the codes submitted to payers for claims processing, it is essential that your processes, systems and reporting are upgraded to accommodate the new code structure. Under ICD-9, codes range from three to five digits while diagnosis coding under the ICD-10 system uses three to seven digits. The expanded number of characters of the ICD-10 diagnosis codes provides greater specificity to identify disease etiology, anatomic site, and severity. Because these additional digits allow for more information to be conveyed in a code, providers will need to enhance their documentation to include the additional detail needed for proper code assignment. For example, most ICD-10 codes contain digits not required in the ICD-9 code set such as:
• exact location, e.g exact digit/limb
• laterality
• comorbidity and comortality
• cause of injury/illness
• severity
• episode of care
• location of patient at time of injury
Payers are also operating under the same deadline as providers for this implementation and must be able to accept and process ICD-10 codes for services rendered on and after October 1, 2015. Business processes, claims edits, quality measures, medical review policies, and payment calculations are a few of the contributing processes and systems that require revamping to accommodate the new codes, adjudicate claims, and communicate payment results.
Affinity Revenue Services can assist your office with this major transition to ensure compliance and eliminate any lapse in payments.
Preparation for ICD-10 at Affinity Revenue Services began years ago, with the majority of the basic programming changes completed that will allow us to electronically receive, process and transmit the increased number and length of ICD-10 codes under this new coding structure. We have completed end-to-end testing with current clients’ facilities to ensure the successful transfer of data for processing and billing. Testing with payers has also been coordinated to ensure they can receive and process our claims correctly and continue providing explanation of payment.
We provide overall business consulting support to physicians and surgeons in private practice. Whether the need is ICD-10/Stage 2 Meaningful Use EHR/EMR systems, comprehensive medical billing solutions to optimize revenue cycle, or electronic filing of patient files, we have solutions to assist in every facet of a physician’s practice.
Affinity Revenue Services will provide updates to clients on industry communications and information related to the transition of this next generation of diagnosis coding as we move through the implementation period. At this time if you have any preliminary questions or concerns, please feel free to contact one of our knowledgeable coding compliance team members at 855-592-9222, or email info@affinityrs.com today.
Check Also
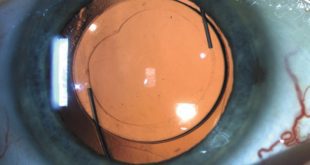
CUSTOMIZABLE LIGHT ADJUSTABLE LENS A GAMECHANGER FOR CATARACTS PATIENTS
All Americans have some degree of cataract change by the age of 75. As the …
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages