There are multiple types of breast cancer, and it affects both men and women. Importantly, the statistics of survival are increasing, mostly due to patient education and early diagnosis. In the United States, the CDC reports that over 276,400 women are diagnosed with invasive breast cancer annually, along with 48,530 new non-invasive breast cancer cases. Breast cancer also affects approximately 2,600 men each year.
There are multiple types of breast cancer, and it affects both men and women. Importantly, the statistics of survival are increasing, mostly due to patient education and early diagnosis. In the United States, the CDC reports that over 276,400 women are diagnosed with invasive breast cancer annually, along with 48,530 new non-invasive breast cancer cases. Breast cancer also affects approximately 2,600 men each year.
We caught up with BayCare’s Breast Surgical Oncologist, Dr. Lago Toro, to find out more about the importance of early diagnosis, genetic testing, and risk factors.
Imaging
I encourage patients to get a mammogram yearly, and if they are high risk or have had breast cancer before, they ideally should be screened for high risk. High risk screening entails mammograms and MRIs on a yearly basis but staggered every six months along with a clinical breast exam. Many patients have dense breast tissue, making it challenging to accurately diagnose them with traditional mammography. High risk screening allows for a more in depth exam of the breast tissue.
Screening Recommendations
The American Society of Breast Surgeons recommends, women less than 25 years of age should undergo formal risk assessment for breast cancer. Women with an average risk of breast cancer should initiate yearly screening mammography at age 40. Women with a higher-than-average risk of breast cancer should undergo annual screening mammography as well as offered yearly supplemental imaging, such as MRI; this screening should be initiated at a risk-based age. The MRI and Mammography can be alternated every six months for those with any high-risk factors.
The Role of Genetics and Other Risk Factors
Genetic risk factors and breast malignancies require multi-panel genetic testing. Multi-panel testing is a type of genetic testing that looks for mutations in several genes at once. A family or personal history of breast or other cancers, as well as specific hereditary genetic mutations, can leave you at a significantly higher risk of developing breast and different types of cancer. The multi-panel genetic testing, regardless of sex, can facilitate early diagnosis and increase survival rates.
We do genetic testing in our office. If there is a first-degree family history, for example, if a mother or sister was diagnosed at age 40, we recommend that the patient start screening mammograms ten years prior to their family member’s age of diagnosis. While I believe at home exams are important, it’s critical to have a clinical physical examination with your OB/GYN or PCP, since they can palpate and find early signs and lumps to facilitate the patient’s imaging needs. Early diagnosis stipulates a 97% survival rate.
Some of the symptoms to look for are palpable masses around the breast and the armpit region, nipple discharge (especially spontaneous), skin changes, dimpling, pain and nipple retraction.
Biopsy and Treatment
If an abnormality is detected on imaging, we are able to perform a minimally invasive biopsy (ultrasound-guided core biopsy, stereotactic core biopsy, or MR-guided core biopsy) procedure that uses image-guidance to see if the abnormality is benign or malignant.
Not every benign lesion needs to be surgically removed. There are multiple options for cancer treatment nowadays. Some include lumpectomy, which conserves the breast and can be performed with hidden scar breast surgery. There are also different types of mastectomies performed as well as immediate reconstructions. If we need to treat the malignancy with radiation, there are different options. The traditional radiation includes energy delivered to the breast in a sequential fashion for a period of a few weeks. An alternative in some cases, is accelerated partial breast irradiation or brachytherapy. Brachytherapy allows the radiation energy to be directly targeted to the lumpectomy bed. This is done through a catheter that I place under ultrasound-guidance in the office. The catheter has chambers in which the radiation seeds are funneled through. The procedure takes about five days, twice a day treatment.
Diagnosis and Screenings
Mammograms help diagnose breast cancer at an earlier stage and save lives; eliminating metastasizing cancer and deaths. However, not all breast cancers are detected with mammography. It’s critical to speak to your doctor about which options are best for you.
It’s also very important to continue with screening mammograms and MRIs during this COVID-19 pandemic. We are open for screening and diagnostic studies. Breast health is important and we are here to help. We’re taking all CDC precautions to screen and sanitize to keep your safety as a priority.
Don’t wait, schedule your appointment today.
It’s easy to schedule a screening mammogram or other imaging exams, such as a CT, MRI, ultrasound or X-ray online at baycare.org or by calling (855) 269-4333.
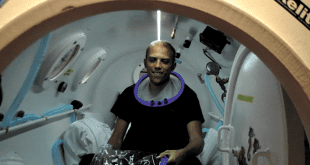
Claudia Lago Toro, MD, Breast Surgical Oncologist
Claudia Lago Toro, MD, is board certified in general surgery. She received her Doctorate in Medicine from the University of Puerto Rico School of Medicine in San Juan, Puerto Rico. She followed that up with a general surgery residency at Baystate Medical Center the Western Campus for Tufts Medical School in Springfield, Massachusetts. Dr. Lago Toro continued her medical education by completing a breast surgical oncology fellowship at Bryn Mawr Hospital in Bryn Mawr, Pennsylvania. As a breast surgical oncologist, she treats male and female breast cancer patients, as well as those with benign breast disease. She has been chosen by her peers as TopDoc in Tampa a few years in a row. Dr. Lago Toro has extensive experience in minimally invasive breast biopsies, mastectomies, including nipple-sparing approach and the administration of breast brachytherapy for radiation therapy. She is also certified in hidden scar breast surgery and performs nipple-sparing mastectomies. Her clinical interests include patient education and creating awareness of breast cancer, and she has served as a resident clinical educator at Tufts University in Boston, Massachusetts. Dr. Lago Toro is a member of the American Society of Breast Surgeons, the Society of Surgical Oncology and the American Society of Clinical Oncology.
BayCare Medical Group Breast Surgery
at St. Joseph’s Women’s Hospital
4321 N Macdill Ave Ste 203
Tampa, FL 33607
Phone: (813) 873-7615
BayCare Medical Group Breast Surgery
at St. Joseph’s Hospital – North
4211 Van Dyke Rd, Ste 200
Lutz, FL 33558
Phone: (813)- 873- 7615
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages