 January is Glaucoma Awareness Month, dedicated to helping people understand what glaucoma is, how to catch it before it causes serious vision damage, and the treatment options available for people with additional issues like cataracts.
January is Glaucoma Awareness Month, dedicated to helping people understand what glaucoma is, how to catch it before it causes serious vision damage, and the treatment options available for people with additional issues like cataracts.
What is Glaucoma?
Glaucoma is a group of eye diseases affecting the optic nerve at the back of the eye. The optic nerve is a complex collection of more than a million nerve fibers that captures and transfers visual images to the brain. Glaucoma prevents proper drainage of fluid from the eye, causing increased pressure that compresses the optic nerve and causes its cells to atrophy and die.
Although glaucoma can occur at any age, but is especially common in people over 60, as well as in people with diabetes, a family history of glaucoma, certain vision problems, very high or low blood pressure and/or African, Asian or Hispanic heritage.
If I Had Glaucoma, I’d Know It…Right?
Not necessarily. In fact, more than 3 million Americans have glaucoma and roughly half of them don’t know it. The reason is because glaucoma’s damage is so subtle and stealthy that 40% of vision can be lost before you notice it. Typically, people begin to experience blind spots in their peripheral vision, which includes side vision as well us overhead and below. Sadly, once vision loss occurs, it is permanent. Due to its stealthy nature, glaucoma is the leading cause of blindness in the US, accounting for roughly 10% of all cases.
Types of Glaucoma
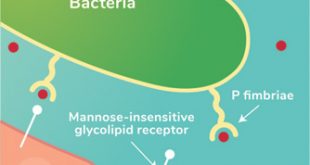
There are two main types of glaucoma: primary open-angle glaucoma, or POAG, which is the most common form, accounting for more than 90% of cases, and angle-closure glaucoma. In healthy eyes, a clear fluid called the aqueous humor provides moisture and nutrients to the eye and then drains out through a microscopic drainage channel called an “angle.” In people with POAG, the aqueous humor doesn’t drain sufficiently and the excess fluid creates intraocular pressure that damages the optic nerve’s sensitive fibers. “Once the nerve fibers are damaged, there is a loss of peripheral vision,” says Lake Eye ophthalmologist and eye surgeon Dr. Vinay Gutti. “From there, this tunnel vision can lead to total blindness.”
In narrow angle glaucoma, the drainage channel may be blocked and/or the aqueous fluid can’t reach it and remains in the eye, which also places pressure on the optic nerve. Unlike most types of glaucoma, narrow angle glaucoma can produce sudden and alarming symptoms like eye pain, light halos, headache, vision loss, nausea and vomiting that may remain or subside and recur again later. Anyone experiencing symptoms like these should see a doctor immediately, even if it means going to the ER.
Secondary glaucoma refers to glaucoma that is caused or exacerbated by another condition or occurrence, such as injury to the eye, inflammation, diabetes, steroids and certain other drugs, and advanced cases of cataracts.
Can Glaucoma Be Cured?
We haven’t yet discovered a cure for glaucoma, but advances in medicine, science and technology are revolutionizing the way glaucoma is treated. Once the type of glaucoma is diagnosed, there are proven ways to treat glaucoma that can delay or arrest its progression before it causes serious, permanent damage.
The best way to manage glaucoma is to catch it early, and luckily that’s easy to accomplish. Regular comprehensive eye exams administered by your ophthalmologist or optometrist can determine if you have glaucoma. Having regular check-ups, even if you don’t have symptoms, can help ensure the disease is caught early, when it can be effectively treated. It is recommended that you have at least one comprehensive eye exam by age 40 (or 35 if you’re in a higher risk group) and every two to three years afterward. Once you reach age 60, we recommend an annual eye exam. Exams are quick, safe and painless, so there’s no reason not to make them part of your routine healthcare plan.
What Treatments are Available?
In most cases, prescription eye drops designed to reduce intraocular pressure are enough to arrest glaucoma’s progress and protect vision. Other cases may respond to adding specific oral medication(s).
Open-angle Glaucoma
Most patients with open-angle glaucoma respond favorably to Selective Laser Trabeculoplasty, or SLT, a safe, quick and painless laser procedure designed to provide long-term relief from excess eye pressure. Performing SLT, your Lake Eye ophthalmologist uses a microscope to direct a mild, specialized light directly to the eye’s drainage channel, encouraging it to open and expel fluid and pressure more normally. Performed in your doctor’s office in about 10 minutes, SLT significantly lowers eye pressure in more than 80% of patients. After SLT, many patients are able to reduce their use of glaucoma eye drops and medications. About half of SLT patients require one or more follow-up treatments, with ultimate results typically lasting from 2-5 years.
Glaucoma and Cataracts
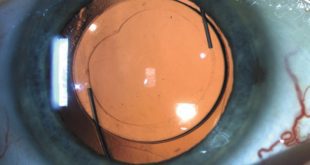
Glaucoma patients with cataracts can have their glaucoma effectively treated using a procedure performed during the same surgical session as cataract removal and lens replacement. One option is the Hydrus® Microstent, an innovative device that your Lake Eye surgeon can insert into a tiny vessel in the eye called Schlemm’s canal, a port that sends vitreous humor back into the body’s circulatory system. The Hydrus Microstent immediately promotes normal fluid outflow, reducing eye pressure and enabling most patients to reduce or eliminate their dependence on glaucoma medication. “The Hydrus Microstent widens the natural drainage system of the eye, encouraging expulsion of fluid and relieving pressure,” says ophthalmologist and eye surgeon Dr. Scot Holman. “The mircostent is miniscule, about the size of an eyelash, and is implanted using microscopic incisions that heal rapidly with little risk of complication. And because we install it via the same corneal incision we use for cataract surgery, it’s safe and convenient for patients and requires minimal healing time.”
Outcomes show that 3 out of 4 Hydrus Microstent patients experience a significant reduction in eye pressure compared to those having cataract surgery only, and most don’t need eye drops two years following implantation.
Other exciting options for cataract patients with mild to moderate POAG are the iStent® and iStent inject® Trabecular Micro-Bypass implants. The iStent works to open up the eye’s natural drainage system and keep it open for months to come. The iStent inject contains two microscopic stents and is suitable for people whose condition requires extra drainage facilitation. 20,000 times smaller than an intraocular lens, these FDA-approved medical implants reduce excess fluid and lower eye pressure so effectively that patients can often stop or reduce their glaucoma medication for an entire year following surgery.
“The iStent inject allows most patients to achieve healthy eye pressure and reduce or cease their dependence on eye drops,” says ophthalmologist and eye surgeon Dr. Scott Wehrly. “These implants are placed during the same procedure as cataract removal and can greatly limit and even prevent further vision damage from glaucoma.”
The Hydrus Microstent, iStent and iStent inject are not appropriate for everyone, including patients with primary- or secondary-angle-closure glaucoma. If you have glaucoma and are planning cataract surgery, ask your ophthalmologist or optometrist if these revolutionary technologies might be right for your condition. You may find yourself experiencing clearer, healthier vision in no time.
Lake Eye Associates
352-750-2020
www.lakeeye.com
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages