By Bo Martinsen, MD
Experts saw this pandemic coming.
Already in the 1990s – and throughout the last two decades – scientists repeatedly warned us about the increasing likelihood of global pandemics.
Now that COVID-19 has arrived, many efforts feel like too little, too late. But there are still things that we can do to mitigate damage. One of them includes mobilizing “specialized forces” that are key to resisting, surviving, and recovering from infections.
I am talking about the microbiome.
How Does Gut Health Affect the Immune System?
One of the most astounding recent developments in medicine is the notion that our gut bacteria (also known as the microbiome) control our immune system and susceptibility to chronic illnesses.
But the microbiome also influences our vulnerability to infection.
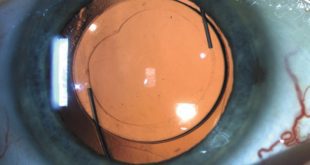
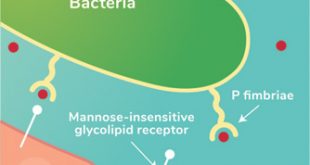
Starting from birth, our gut bacteria develop a fascinating collaboration with our immune cells. When harmful pathogens make their way into our digestive system, our gut bacteria are at the frontlines. They combat pathogenic bacteria and viruses by competing with them for nutrients and adhesion sites, releasing toxins to prevent these bad actors from taking hold, and by signaling our immune cells into action.
What Is Dysbiosis?
Because of this relationship between the immune cells and our microbiome, it’s critical to foster a varied, healthy composition of bacteria throughout life. It comes as no surprise that dysbiosis – or having a poor microbial balance – is linked to most illnesses and health outcomes.
The two highest risk factors for dying from infections are advanced age and having a pre-existing, poorly controlled chronic illness. In both of these scenarios, dysbiosis plays a role.
How to Improve Our Gut Health
While we can’t change our age, we can certainly improve gut health through a variety of means:
Eating a Balanced Diet
There is an old saying that we are what we eat. And if you consider what diet does to the microbiome, this makes sense: We harbor the types of bacteria that favor our food and lifestyle.
Western diets – which are typically low in fiber and saturated with refined sugars and the wrong kinds of fats – are especially appreciated by bacteria that send out inflammation-stimulating and intestinal-wall destroying substances. When we consume these kinds of diets, it nourishes these inflammation-driving bacteria at the expense of our ally microbes.
The consequence is that the immune system is already over-challenged and worn out, with little ability to fight new infections from pathogenic viruses or bacteria.
Poor nutrition status is almost always linked to poor health outcomes for any disease. While history has repeatedly acknowledged the importance of getting the right nutrients, it is disheartening that we have developed a society that frequently undermines this fact. Even in hospitals, where people are most at risk and need the highest quality diet, patients are typically offered poor-quality, pro-inflammatory foods.
Numerous studies are now exploring the role of probiotics for restoring a healthy microbiome. But perhaps most important of all is increasing our intake of beneficial fibers from whole foods like oats, nuts, lentils, beans, fruits, and vegetables.
Additionally, getting enough omega-3s is also important for maintaining a good balance of gut bacteria.
Having a Healthier Lifestyle
The health of our microbiome is not just diet-dependent. Lifestyle factors – like exercise and exposure to sunshine – also have positive microbiome-regulating abilities. For instance, studies in humans and mice show that aerobic exercise can increase microbial diversity in the gut.
In contrast, behaviors like smoking, drinking alcohol, and unnecessary antibiotic use are associated with poor microbial health. An estimated 30% of antibiotics given to children are not medically necessary. This is especially disturbing since antibiotic misuse can have long-term negative effects on the microbiome.
Getting Enough Sleep
Sleep is another lifestyle factor that has a profound effect on our resident bacteria. Studies reveal that changes in our sleep pattern (as well as sleep deprivation) can disturb the diversity and composition of our microbiome. This connection could partly explain why health care workers who work night shifts are more susceptible to respiratory infections than those who do not work during the night.
Mice studies indicate that melatonin supplementation also increases microbial diversity and promotes a healthier balance of gut bacteria. This connection has led scientists to theorize that the beneficial effects of melatonin may be partially due to this molecule’s microbiome-regulating abilities.
For the full article and references, please visit:
https://omega3innovations.com/blog/how-your-gut-health-influences-your-immune-system/
About Bo Martinsen, MD
Dr. Martinsen is an omega-3 specialist, innovator, and advocate for natural foods. As co-founder and CEO of Omega3 Innovations, he has created several medical food products that combine effective doses of omega-3s with soluble fibers and other nutrients. Before Omega3 Innovations, Dr. Martinsen practiced medicine in Norway for 20 years.
Call Us: 941-485-4400
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages