By Joseph Borrelli, Jr., MD, MBA
The Center for Disease Control (CDC) estimates that there are approximately 55 million Americans with arthritis, and this is projected to increase to 78 million by the year 2040. The most common type of arthritis is osteoarthritis (OA), osteoarthritis is also commonly referred to as “wear and tear arthritis” and “degenerative joint disease”. The knee is one of the most common of the body’s large joint to develop OA.
What is OA?
Osteoarthritis is a condition where the natural cushioning substance, articular cartilage, that covers the ends of each bone in a joint, is gradually worn away. Articular cartilage is a meticulously organized and is a very tough material, it consists of chondrocytes (the cells of the cartilage), collagen (the fiber of the cartilage), proteoglycans (large bottle brush molecules which attract and trap water) and water. There are no nerve ends or blood vessels within cartilage, which impairs its ability to repair itself once degeneration starts.
The common denominator in the development of OA is the wearing away of the articular cartilage of our joints. Some joints appear to be more susceptible to the development of OA (knee) than other joints (elbow). Generally, as the articular cartilage begins to wear away, tiny cartilage particles are released into the joint’s fluid and are taken up by the synovial cells of the lining of each joint. The take-up of these cartilage fragments stimulates an inflammatory response within the joint, which is responsible for many of the symptoms we experience once OA begins to set in.
OA Symptoms:
• Soreness and pain
• Joint swelling and stiffness
• Warmth
• Mobility issues
It is not uncommon for these symptoms to persist and worsen over the course of years, eventually leading to loss of joint motion, deformity and functional limitations.
Diagnosing OA
Correctly diagnosing OA is important so as to make sure the joint symptoms are not caused by more sinister conditions (infection, fracture, tumor, etc.). Generally, OA can be diagnosed based upon a thorough history and physical examine and regular x-rays. Occasionally, more high-tech imaging is necessary to confidently make the diagnosis of OA. These more sophisticated imaging technics include CT scans and on occasion Magnetic Resonance Imaging (MRI). In most cause MRI’s are not necessary for the diagnosis of OA and should be reserved for those situations where the diagnosis is unclear.
Treatment Options
Once OA has been definitively diagnosed treatment can be initiated. In most cases treatment of OA during its early stages includes the use of acetaminophen, ice, weight reduction and muscle strengthening. Muscle strengthening, particularly the muscles around the knee, should be performed under the supervision of a certified physical therapist to assure the exercises are performed correctly and to reduce the risk of addition injury. The muscles about the knee are secondary stabilizers and their strengthening can help reverse the instability that commonly occurs with thinning of the articular cartilage, ligamentous laxity and generalized muscle atrophy that occurs as we age and become less active. The use of acetaminophen, weight reduction, ice and physical therapy are the primary components of the first stage of conservative management of OA of the knee.
If the above measures are unsuccessful in relieving the knee pain associated with OA, additional measures can be undertaken. These include judicial use of non-steroidal anti-inflammatory drugs (NSAIDS) like ibuprofen, naproxen and diclofenac, to mention just a few. NASIDS are designed to reduce the inflammation associated with OA thereby reducing the pain and swelling of the degenerating and inflamed joint. Although effective in relieving the symptoms of OA, particularly in its early stages, NSAIDS have been associated with gastric upset, stomach ulcers and kidney problems. The newer NSAIDS that have recently become available are more specific inhibitors of the enzymes involved in inflammation and are less likely to interfere with the protective lining of the GI tract. These newer NSAIDS are also taken less often then the older NSAIDS, during the course of the day. Although for many patients these medications are very effective at relieving their symptoms of OA they have not been shown to affect the natural history of the disease process.
The third line of treatment for degenerative arthritis of the knee is intra-articular injections. Typically, the first injections performed include a combination of fast and delayed action analgesics (lidocaine) combined with a corticosteroid. These types of injections are typically effective early in the disease process for relieving the pain and swelling of the knee. However, subsequent injections seem to be less and less effective at relieving pain and swelling of the knee. This type of injection is designed to numb the knee (analgesics) and reduce the surrounding inflammation (corticosteroids). The effects of these injections is somewhat unpredictable with some patients getting several months’ worth of pain relief and other patients getting only a few weeks of pain relief. The length of time this type of injection is effective is related to the arthritic stage of the knee.
Visco-supplementation of the knee’s synovial fluid is another type of knee injection. These, mostly hyaluronic acid products are designed to increase the lubrication of the knee and provide anti-inflammatory action, both which aid in pain reduction. These products can be quite expensive and often require pre-authorization by one’s insurance company before being administered by your physician but can provide long lasting pain relief.
Cooled radiofrequency ablation (COOLIEF) treatment of the knee is generally reserved for knee pain, secondary to advanced OA, in patients who are unable or unwilling to undergo a total knee arthroplasty (TKA). This procedure is generally performed by an interventional radiologist and involves temporarily incapacitating the nerves around the knee that are responsible for transmitting pain. Pain relief from this procedure is possible for up to a year or more.
Some Individuals Will Need Knee Replacement
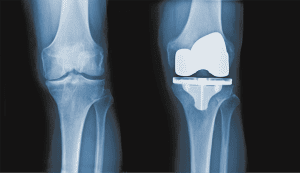
Once all means of conservative management for OA of the knee have been exhausted consideration can be given to performing a total knee replacement/TKA. The goals of TKAs is to relieve pain, improve function and to correct leg deformity and increase knee range of motion. This surgical procedure involves removing the arthritic surfaces of the femur, tibia and patella and resurface them with metal and plastic. In most cases, the total knee components are cemented or glued into place with an acrylic cement, doing so allows the patient to weight-bear on the prosthesis once the patient has recovered from anesthesia. In general, total knee replacements have an excellent track record and, in most cases, provide excellent pain relief and improved function for many years and in some cases decades.
Although there are several different types of total knee prostheses on the market, I prefer the use of a prosthesis that does not rely on the anterior cruciate or posterior cruciate ligaments for stability, but rather relies on the design and the fit of the prosthesis for its stability and function. This particular type of design, the “medial pivot” or “medial congruity” prosthesis is being recognized more and more by experts in the field as the best design for primary TKA. This design has been shown to allow easier and more consistent implantation, improved knee range of motion, improved stability and less post-operative anterior knee pain, as compared to other types. Additionally, these “medial pivot” types have recently been shown to have superior longevity, including a recent report where nearly 98% of these knees were still in place at 18 years.
Although, there have been significant improvements in the design and manufacturing of total knee replacement components this type of surgery is not without risks and potential complications. Before a decision to undergo a total knee replacement is made, patients should have exhausted all means of conservative management for their knee arthritis. Prior to surgical intervention patients should have a thorough discussion of the procedure and of the patient’s expectations, as well as a complete review of the potential surgical risks, with their surgeon. Additionally, in an effort to minimize these risks and maximize outcomes patients should be medically optimized (including weight reduction, diabetes control, smoking cessation). Although undergoing a total knee arthroplasty for the treatment of disabling knee arthritis can be a positive life-changing event it is not without risks and requires hard work on the side of the surgeon as well as the patient.
Joseph Borrelli, Jr., MD, MBA is a Board Certified orthopedic surgeon who has been in clinical practice for more than 25 years. Dr. Borrelli received his medical degree from the University of South Florida, Morsani College of Medicine, Tampa, FL. He completed his 5-year orthopedic surgery residency at the world renown Hospital for Special Surgery, Weill College of Medicine, Cornell University, NY, NY. Following his residency, Dr. Borrelli returned to Tampa for completion of an orthopedic trauma fellowship at Tampa General Hospital/USF, Tampa, FL. During his 25 years in practice, he has treated thousands of patients with a variety of fractures, sprains and strains, as well as patients with OA involving the knee, hip, elbow and shoulders. He has previously received awards for his innovative research, teaching and compassionate patient care. Dr. Borrelli is part of BayCare Medical Group and sees patients at the BayCare Outpatient Imaging Center in Trinity, FL and performs surgery exclusively at Morton Plant North Bay Hospital in New Port Richey, FL.
BayCare Medical Group
To schedule a consultation please call (813) 264-6490.
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages