Every year in the United States nearly 800,000 people will suffer from a stroke, also referred to as a cerebrovascular accident (CVA). If it’s not caught early enough, it can lead to death, paralysis, cognitive impairment, aphasia, and many more complications. Stroke prevention cannot be stressed enough, and knowing the signs and symptoms is crucial.
Every year in the United States nearly 800,000 people will suffer from a stroke, also referred to as a cerebrovascular accident (CVA). If it’s not caught early enough, it can lead to death, paralysis, cognitive impairment, aphasia, and many more complications. Stroke prevention cannot be stressed enough, and knowing the signs and symptoms is crucial.
Heather Schweizer, DO, is a neurohospitalist who specializes in diagnosing and treating injuries and diseases that affect the various components of the human nervous system (brain, spinal cord and nerves) while placing an emphasis on evaluating the entire nervous system as a whole in order to identify the root cause of the patient’s ailment. We caught up with Dr. Schweizer of Central Florida Health to find out more.
Q: As a neurologist/neurohospitalist, please explain your role in managing a stroke patient.
A: My role as a neurohospitalist is at the forefront of stroke management from the moment the stroke patient comes in our doors till they are discharged. I am paged the moment a “stroke alert” is called and I meet the patient in the emergency department (ED) to assess them along with the ED physician. We say in stroke care that “time is brain” because when an acute stroke is in progress, a patient is losing 2 million brain cells per minute! We have to assess the patient’s status and history as quickly as possible to administer tissue plasminogen activator (tPA) medication to bust or break apart the clot. This important treatment can essentially save the region of the brain that the stroke is affecting by clearing the clot and restoring blood flow.
The sooner we are able to initiate administration of this medication, if applicable, the more brain we save. And if a patient is found to have symptoms which indicate they have a very large occlusion we may decide to start this clot-busting medication and at the same time transport the patient via helicopter to the University of Florida Health Shands Medical Center, our comprehensive stroke receiving partner hospital for clot retrieval.
After the initial stroke assessment and treatment, I will provide daily hospital care for the stroke patient and we will perform various diagnostic tests to assess why they had a stroke. Their carotid arteries are assessed for stenosis, the heart is assessed with an echocardiogram, and the patient is continually monitored via telemetry to make sure they do not have an arrhythmia, such as atrial fibrillation, which is another cause of stroke. If we can hone in on the “why” of their particular stroke process, then we can better pinpoint the most optimal medication to give them for prevention of another stroke. I always tell my patients that once we are past the initial stroke assessment and emergent phase the two treatments for any transient ischemic attack (TIA) or stroke are 1) rehabilitation for residual deficits (physical , speech, occupational or music therapy) and 2) optimizing prevention of developing another TIA or CVA.
And finally, after the patient’s admission for diagnostics and once prevention is optimized, we work closely with the primary internal medicine team, therapy modalities, and case management to place the patient in the most optimal inpatient rehabilitation facility (or outpatient rehabilitation if deficits are minimal) and assure continuity of care with post-hospitalization follow-up appointments with outpatient neurologists.
Q: Tell me about the Code Stroke System and how that helps your response team.
A: The Code Stroke System helps our response team by alerting the whole team that we either have a potential stroke patient on their way in or have presented to the emergency department. Local emergency medical services (EMS) providers are integrated into the system and can also alert this code. We have an overhead page as well as a texting alert system. Once we are alerted, we respond emergently to assure the patient is properly assessed for stroke and possible thrombolysis treatment. The patient is immediately met in the ED by the ED physician and me A computerized tomography (CT) test is ordered immediately as a CT of the head is the most important initial diagnostic test because we need to rule-out a hemorrhagic stroke before giving the patient blood thinners. Hemorrhagic strokes account for 15 percent of all strokes and this is why blood thinners, including aspirin, cannot be given by EMS prior to reaching the hospital. The entire response team is vital to the whole process, from neurohospitalist to lab technologist to CT technologist to EMS and everywhere in between. Therefore, a good alert system assures everyone is on the same page because, again, time is brain!
Q: Can the brain heal itself after a stroke and what can patients expect (rehab, speech, walking, etc.)?
A: This is a very tough question and the best way to answer it is that it varies. It depends on the size of the stroke, whether there was successful thrombolytic/thrombectomy performed, the age of the patient and the presence of other co-morbidities, such as uncontrolled diabetes, heart failure, hypertension, smoking, obesity, etc. It also depends on the patient’s pre-stroke physical condition – did they have dementia, gait disturbance, physical deconditioning prior to having the stroke? All of these factors affect a person’s ability to “heal” their brain after a stroke. It is understood, though, that it is possible for collateral circulation around the area of the affected brain to feed these regions, and also, for regions around the stroke to take over functions that were affected by the dead brain tissue. I have witnessed people with the inability to speak clearly rehabilitate substantially to the point where they could communicate quite well.
Q: Why do you think strokes are on the rise, especially in younger adults?
A: Strokes have definitely been on the rise in young adults. There has actually been a stable decline in rates of stroke in patients over the age of 60 and any increase or reduction of decline may be due to better stroke detection with MRI screening. But there has been an increase in young adult strokes, for sure, and I believe this is due to an increase in modifiable risk factors (i.e., diabetes, obesity, hypertension, hyperlipidemia, smoking). It is also due to increased use of certain recreational drugs – specifically, cocaine and amphetamines. Of course, this includes methamphetamine and street drugs that immediately come to people’s minds, but it also includes amphetamines that can be prescribed, such as Adderall and Vyvanse. Although opioid abuse is still rampant, amphetamines are heavily abused in the young adult population and the effect of abuse can be substantial. Young adults in high school and college take the amphetamines to “help them study” and I have heard patients say that they even trade pills with others in their class or have study sessions where they all take amphetamines and pull all-nighters. It’s a dangerous game they are playing, and stroke is a very real threat. I’ve had patients in their 20’s who I have
treated with subarachnoid hemorrhages secondary to Adderall use. In most cases they are using a prescribed and legal medication.
An Advanced Primary Stroke Center
In 2018, The Villages® Regional Hospital earned recertification and The Joint Commission’s Gold Seal of Approval® for Advanced Certification for Primary Stroke Centers. This also includes the American Heart Association/American Stroke Association’s Heart-Check mark. The Gold Seal of Approval® and the Heart-Check mark represent symbols of quality from their respective organizations.
The Villages® Regional Hospital has been accredited since November 2016 and provides rapid treatment to more than 550 area residents who suffer a stroke annually, offering 24-hour emergent diagnostic and treatment services to patients presenting with acute ischemic stroke and other neurovascular disorders.
The Villages® Regional Hospital
www.TheVillagesRegionalHospital.org
1451 El Camino Real, The Villages, FL 32159
Check Also
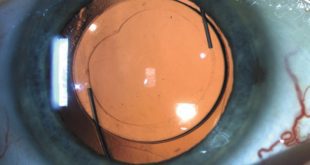
CUSTOMIZABLE LIGHT ADJUSTABLE LENS A GAMECHANGER FOR CATARACTS PATIENTS
All Americans have some degree of cataract change by the age of 75. As the …
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages