By Tom Tran PA-C, MPAs, NCCPA Surgery Board Certified –
 Do your legs often feel heavy, restless, or painful; or are they covered with varicose or spider veins? If so, you may be one of the many people walking around with venous insufficiency and not even know it. Unfortunately, venous insufficiency is often under diagnosed and under treated. Continue reading to learn more about chronic venous insufficiency, a condition that may be affecting you or someone you know.
Do your legs often feel heavy, restless, or painful; or are they covered with varicose or spider veins? If so, you may be one of the many people walking around with venous insufficiency and not even know it. Unfortunately, venous insufficiency is often under diagnosed and under treated. Continue reading to learn more about chronic venous insufficiency, a condition that may be affecting you or someone you know.
When your leg veins cannot pump enough blood back to your heart, you have chronic venous insufficiency (CVI). CVI is also sometimes called chronic venous disease, or CVD. You have three kinds of veins: superficial veins, which lie close to the skin, deep veins, which lie in groups of muscles, and perforating veins, which connect the superficial to the deep veins. Deep veins lead to the vena cava, your body’s largest vein, which runs directly to your heart.
When you are in the upright position, the blood in your leg veins must go against gravity to return to your heart. To accomplish this, your leg muscles squeeze the deep veins of your legs and feet to help move blood back to your heart. One-way flaps, called valves, in your veins keep blood flowing in the right direction. When your leg muscles relax, the valves inside your veins close. This prevents blood from flowing in reverse, back down the legs. The entire process of sending blood back to the heart is called the venous pump.
When you walk and your leg muscles squeeze, the venous pump works well. But when you sit or stand, especially for a long time, the blood in your leg veins can pool and increase the venous blood pressure. Deep veins and perforating veins are usually able to withstand short periods of increased pressures. However, sitting or standing for a long time can stretch vein walls because they are flexible. Over time, in susceptible individuals, this can weaken the walls of the veins and damage the vein valves, causing CVI.
What causes Chronic Venous Insufficiency?
Over the long-term, blood pressure that is higher than normal inside your leg veins causes CVI. This can lead to damage to the valves, which can further worsen the problem. In some instances, the valves that prevent blood from flowing “backwards,” can be congenitally defective. Other causes of CVI include deep vein thrombosis (DVT) and phlebitis, both of which cause elevated pressure in your veins by obstructing the free flow of blood through the veins.
DVT occurs when a blood clot (properly called a thrombus) blocks blood from flowing toward the heart, out of a deep or perforating vein. The blood trying to pass through the blocked veins can increase the blood pressure in the vein, which, in turn, overloads your valves. Vein valves that do not work properly are called incompetent because they stretch and no longer work efficiently, and incompetent valves contribute to CVI. DVT is a potentially serious condition that causes leg swelling and requires immediate medical attention because sometimes the blood clots in the veins can break off and travel to the lungs. This condition is called a pulmonary embolus.
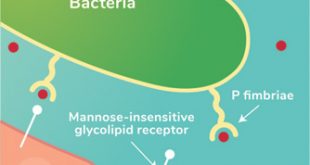
Phlebitis occurs when a superficial or deep vein becomes swollen and inflamed. This inflammation causes a blood clot to form, which can also lead to DVT.
Factors that can increase your risk for CVI include a family history of varicose veins, being overweight, being pregnant, not exercising enough, smoking, and standing or sitting for long periods of time. Although CVI can affect anyone, your age and sex can also be factors that may increase your tendency to develop CVI; women older than 50 most often get CVI.
Symptoms of Chronic Venous Insufficiency
If you have CVI, your ankles may swell and your calves may feel tight. Your legs may also feel heavy, tired, restless, or achy. You may feel pain while walking or shortly after stopping.
CVI is also associated with varicose veins. Varicose veins are swollen veins that you can see through the skin. They often look blue, bulging, and twisted. Large varicose veins can lead to skin changes like rashes, redness, and sores.
CVI can also cause problems with leg swelling because of the pressure of the blood pooling in the veins. Your lymphatic system may also produce fluid, called lymph, to compensate for CVI. Your leg tissues may then absorb some of this fluid, which can increase the tendency for your legs to swell. In severe cases, CVI and the leg swelling can cause ulcers to form on the lower parts of the leg.
CVI is one of the oldest ailments known to mankind. Recent discoveries in medicine have shown that in some cases of CVI, there is a major contribution to the condition from superficial veins, which are most often varicose. Patients whose condition is due primarily to incompetence of the perforating veins can be treated by foam sclerotherapy, laser, and radio frequency ablation of such veins.
If you are walking around with painful, restless, swollen legs or have unsightly and bothersome varicose veins, call the Comprehensive Vein Center at 352-259-5960 to learn more about the non-medication treatments that are available. Don’t let your venous insufficiency problem go undiagnosed and untreated any longer!
Source: Society of Vascular Surgery
(352) 259.5960
1050 Old Camp Road Suite 202,
The Villages, FL 32162
2754 Dora Avenue
Tavares, FL 32278
Check Also
Recurrent UTIs: Addressing the Risk of Antibiotic Resistance
Urinary tract infections (UTIs) are common bacterial infections that affect millions of individuals worldwide each …
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages