By Uzoma Nwaubani, MD, FACOG
 The problem of female incontinence and female Pelvic Organ Prolapse (POP) is as old as humanity itself. Sadly, however, it remains hugely under reported. Just the fact that one is of the female gender is in itself a risk factor. Therefore, contrary to popular belief, the incidence of female incontinence and prolapse is not unusual.
The problem of female incontinence and female Pelvic Organ Prolapse (POP) is as old as humanity itself. Sadly, however, it remains hugely under reported. Just the fact that one is of the female gender is in itself a risk factor. Therefore, contrary to popular belief, the incidence of female incontinence and prolapse is not unusual.
Statistically, by age 50, 50% of women have experienced some of these symptoms at least once; by age 70, it could be as high as 70%. If you are experiencing symptoms attributable to them, you’re not alone. Despite these staggering statistics, about 80% of women experiencing incontinence and/or prolapse hide the problem and, instead of seeking medical advice, resort to limiting themselves and, consequently, diminishing their quality of life. This is partly due to societal myths, as well as lack of awareness that urinary incontinence and prolapse can be treated quite effectively.
Both conditions, intimately related to a woman’s sexuality and femininity, can be interrelated and most times go hand in hand. The progressive loss of vaginal support that usually starts with the first pregnancy, culminating with menopausal estrogen deprivation is most times, the underlying cause.
Last month we focused on urinary incontinence, we want to use this article to shed some light on Pelvic Prolapse.
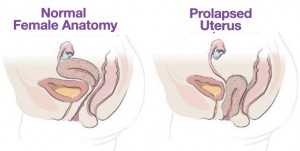
The uterus is held in position by pelvic muscles, ligaments and other tissues. If the uterus drops out of its normal position, this is called prolapse. Prolapse is defined as a body part falling or slipping out of position. Prolapse happens when the pelvic muscles and connective tissues weaken. The uterus can slip to the extent that it drops partially into the vagina and creates a noticeable lump or bulge. This is called incomplete prolapse. Complete prolapse occurs when the uterus slips to such a degree that some uterine tissue is outside the vagina.
Pelvic prolapse is usually accompanied by some degree of vaginal vault prolapse. Vaginal vault prolapse occurs when the upper part of the vagina loses its shape and sags into the vaginal canal or outside the vagina. Pelvic prolapse may also involve sagging or slipping of other pelvic organs, including the bladder, the urethra which is the tube next to the vagina that allows urine to leave your body, and rectum.
Prolapse Repair/Vaginal Reconstruction
Pelvic Organ Prolapse (POP), refers to a group of pelvic problems resulting primarily due to partial or complete loss of pelvic organ support an includes the following:
1. Cystocele (Dropped bladder)
2. Rectocele (Dropped rectum)
3. Vault Prolapse(Dropped upper end of vagina)
4. Enterocele (Dropped intestines through the vaginal wall)
5. Perineocele (Weakened perineal body with ballooning out of the bicycle seat area)
6. Utero-vaginal Prolapse (Dropped cervix and uterus)
7. A combination of some or all of the above
These conditions may be treated conservatively or with surgery. Surgical treatment can be achieved vaginally, laparoscopically, or through an open incision.
Since the underlying factor common to all the above is loss of vaginal wall support, reconstructing this support is important in achieving prolonged post-surgical resolution of symptoms.
This reconstructive process may be achieved in one surgery session. However, sometimes two or more surgical sessions may be necessary to achieve complete restitution of the vaginal integrity and anatomy.
Goals of surgical reconstruction include:
1. Identify and repair the vaginal defect and return the pelvic organs supported by the vagina to as near normal anatomy and function as possible.
2. Restore normal vaginal anatomy
3. Help the patient return to normal vaginal sexual function and gratification
4. Treat any associated urinary or fecal dysfunctions that hitherto may have resulted from the condition
The sub-specialty of Urogynecology, recently renamed “Female Pelvic Medicine and Reconstructive Surgery,” was born to help address this growing need. Female life expectancy in the leading free world averages 89 years and, as such, in any woman’s lifetime, the probability of experiencing any Urogynecological problem is close to 80% (8 OUT OF 10 WOMEN).
In Urogynecology, we evaluate all the structures and systems of the female pelvis, including organs, nerves, ligaments, muscles and blood vessels. Having a well-credentialed and experienced Urogynecologist take care of the very core of your femininity is not just paramount to your health, but is an act of self-love.
At Female Continence & Pelvic Surgery Center, Dr. Nwaubani has one primary objective: to ensure that you live your years in freedom and to their fullest. If you have any questions or concerns, please call 352-633-0703 today and let Dr. Nwaubani help add life to your years!
Felmale Continence & Pelvic Surgery Center
“Add Life To Your Years”
1050 Old Camp Road, Suite 282
The Villages, Fl. 32162
Phone: 352-633-0703 | Fax: 352-633-2232
Tags featured
Check Also
Living with Eczema: New Research Offers Hope Through the KGCD Study
Eczema, also known as atopic dermatitis, affects millions of people worldwide, causing red, itchy, and …
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages



