By Michelle Heine, PA-C, MMS – Ocala Health Neurosurgical Group
 The perception of pain is highly complex not only physiologically but the difference of pain perception between individuals is of great variance. Pain originates primarily from noxious stimuli such as touching a hot stove, being involved in a car accident or spilling acid on the skin. These three examples illustrate the first physiologic process of the perception of pain: transduction. Transduction involves thermal, mechanical or chemical threats to the nervous system, which initiate a cascade of microscopic events leading to the awareness of pain.
The perception of pain is highly complex not only physiologically but the difference of pain perception between individuals is of great variance. Pain originates primarily from noxious stimuli such as touching a hot stove, being involved in a car accident or spilling acid on the skin. These three examples illustrate the first physiologic process of the perception of pain: transduction. Transduction involves thermal, mechanical or chemical threats to the nervous system, which initiate a cascade of microscopic events leading to the awareness of pain.
Most people would agree that pain subsides as the body heals from injury. This is because primary sensory neurons transmit the signal of pain from the noxious stimulus to the brain by a series of action potentials. When the noxious stimulus disappears so does the perception of pain. But what happens when you are left with pain after you have allowed adequate time for your body to heal? Pain without an inciting injury may be the result of damaged peripheral nerves and/or tissues resulting in neuropathic pain.
Damaged primary sensory neurons may become sensitive to the gentlest touch or may even fire without any provocation. This is because injured peripheral nerves may become hyperexcitable leading to out of proportion action potentials traveling to the brain causing pain without a justifiable source. Leaving the patient uncomfortable, frustrated, confused and without hope for relief after exhausting all known resources.
Neuromodulation has been proven effective for treatment of neuropathic pain. Dating back to the 1960s, neurosurgeon C. Norman Shealy was the first to successfully implant a neuromodulation device resulting in liberation from intractable pain. Dr. Shealy’s spinal cord stimulators also known as dorsal column stimulators have significantly advanced since original development. After fifty years of evolution, spinal cord stimulators have become more efficacious, safe and accepted by the chronic pain population.
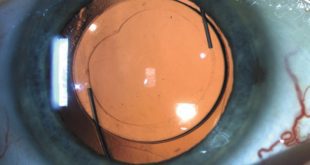
You may be thinking, how does a spinal cord stimulator work? A series of electrodes either in the form of a paddle or a percutaneous lead is implanted above the spinal cord into the epidural space by a neurosurgeon and is connected to a battery also known as a pulse generator. The electrodes deliver a low dose electrical current, which modulates nerve activity, hence the name neuromodulation.
Before permanent implantation, the patient must first pass a spinal cord stimulator trial. This involves sterile placement of electrodes via percutaneous leads performed by a fellowship-trained anesthesia pain physician, physiatrist or neurosurgeon. The leads are secured to the patient’s back by an adhesive dressing and are connected to an external battery also known as an IPG. Working with the patient’s own clinical specialist, different programs are utilized to provide maximum relief from stimulation. After the trial is complete, the patient will be evaluated for determination of trial success. If the trial is deemed successful, permanent implantation will be scheduled.
The patient generally waits a period of time to heal between the trial and permanent implantation. The surgery is fairly quick and straightforward. A permanent lead will be placed in the epidural space of the thoracic spine and the connecting wires are tunneled underneath the skin to the battery site. Incisions are usually closed with dissolvable sutures and special surgical glue. There is typically no need to have sutures or staples removed after surgery. The spinal cord stimulator will not be turned on until two weeks after surgery to ensure proper scarring of the lead placement. The patient must refrain from bending, lifting greater than ten pounds or twisting six weeks post operatively. After six weeks, the patient is released to full activity without restrictions.
Spinal cord stimulators are easily portable with the controller usually the size of an iPhone. The patient may go about their normal routine without having to stop to take a pill in order to experience adequate pain relief. Thus improving quality of life, functionality and mood.
Neuromodulation is not limited to spinal cord stimulation. Deep brain stimulation known as DBS is FDA-approved to treat essential tremor, Parkinson’s disease and dystonia. Vagal nerve stimulation is used to treat obesity, asthma, seizures, and may even be trialed for heart failure. Sacral nerve stimulation is used to treat incontinence and pelvic ailments. Intrathecal pain pumps are used to deliver low-dose medications directly to the source of pain perception, reducing the need for high-dose oral medications.
Neuromodulation is continually advancing with new technology emerging on a daily basis. Currently, scientists are working on a neuromodulatory system utilizing thought to produce movement via a computer, especially appealing to motor-impaired patients. Neuromodulation offers another chance to those who have failed multiple treatment options who present with neuropathic pain.
Ocala Health Summerfield ER
14193 S US HWY 441
Summerfield, FL 34491
Check Also
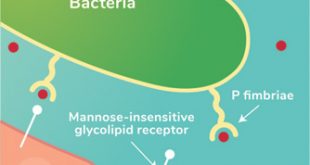
Recurrent UTIs: Addressing the Risk of Antibiotic Resistance
Urinary tract infections (UTIs) are common bacterial infections that affect millions of individuals worldwide each …
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages