By Craig Chappeall, DO, Functional Health and Sports Medicine of Ocala
 Prolotherapy
Prolotherapy
Prolotherapy is an innovative injection technique whose primary intent is to repair connective tissue (ligament, tendon or cartilage) and promote growth of normal cells. Prolotherapy relieves pain by directly impacting the underlying condition causing that pain. In contrast to many medical treatments that may provide only temporary benefits, this safe, proven treatment offers lasting relief.
Performed in a medical office, prolotherapy relieves pain without the risks of surgery, without general anesthesia or hospital stays, and without a prolonged recovery period. In fact, most people return to their jobs or usual activities right after the procedure.
How Does Prolotherapy Work?
Prolotherapy works by stimulating a brief period of inflammation to produce growth factors. Prolotherapy solutions often include dextrose for a growth factor stimulation effect, but the inflammatory signal that result cause a more vigorous growth response. The same type of inflammation that the body uses to repair itself following an injury. However with prolotherapy there is no significant injury, because there is no actual stretching or tearing of fibers. The body then begins a repair process, which allows the structure to become stronger and tighter rather than first becoming weaker and looser.
Effective treatment usually takes between 3 and 6 treatments. Treatments are given approximately once a month. If there is marked improvement after only 1-2 treatments, then no further treatments may be necessary. There is no limit to the number of treatments that may be given, as long as improvement continues to be seen. There is also no increase in risk factors with subsequent treatments.
Prolotherapy is extremely safe, and while there are risks to any injection procedure, the risks are minimal.
How long does it take?
The total appointment time takes approximately 30-60 minutes, including preparation, treatment and recovery time.
What are the expected results?
Initially, mild but temporary swelling and stiffness may occur. Some patients see noticeable improvement after the first sessions are completed, while others realize increasing improvement on each successive visit. Research studies show that over 80 percent of people treated with prolotherapy report a good or excellent result. Many of them are permanently cured. Not only do they enjoy simple pleasures again – a good night’s sleep, sitting through a movie, taking a walk – but many also return to aggressive physical activities.
Common problems treated
• Joint instability, including the knee, shoulder, wrist, ankle, hip and other joints
• Chronic sports injuries
• Osteoarthritis
• Chronic or recurrent tendinitis, such as Tennis elbow, partial rotator cuff tears, Achilles tendinitis or patellar tendinitis.
• Chronic or recurrent sprains & strains of the ligaments and tendons
• Whiplash injuries
• Chronic back pain
Musculoskeletal Ultrasound (MSKUS)
Over the last few years the use of ultrasound in sports and orthopedic medicine has grown rapidly. Now sports medicine physicians are using ultrasound to diagnose injuries and to guide injections making them accurate and effective.
Advantages of Diagnostic
MSKUS MSKUS has many advantages over x-rays, MRI, and CT scans. These include:
• better resolution of soft tissue than MRI
• convenient in-office service; no need to go to another facility
• no exposure to ionizing radiation
• no claustrophobia
• the ability to perform a dynamic or “live” study
• cost-effective
• ability to see inflammation
• ability to guide injections
Ultrasound-Guided Injections
One great advantage of MSKUS is the ability to guide the needle when performing injections. Injections under ultrasound guidance helps ensure accurate needle placement and medication delivery. This improves both patient comfort and treatment efficacy. It also helps avoid placing the needle in nearby dangerous structures such as nerves, blood vessels, or other organs.
Platelet-Rich Plasma Therapy (PRP)
PRP is a rapidly emerging technique and is showing exciting potential with osteoarthritis of the knee, shoulder, hip and spine, rotator cuff tears, chronic plantar fasciitis, anterior cruciate ligament (ACL) injuries, pelvic pain and instability, back and neck injuries, tennis elbow, ankle sprains, tendonitis, and ligament sprains. Most people associate platelets with clot formation. While that certainly is an important function of platelets, they are also very much involved in injury healing. Human platelets are extremely rich in connective tissue growth factors. Injecting these growth factors into damaged ligaments, tendons, and joints stimulates a natural repair process. But in order to benefit from these natural healing proteins, the platelets must first be concentrated. In other words, PRP recreates and stimulates the body’s natural healing process.
How Does PRP Work?
Platelets are a specialized type of blood cell. Blood is made up of 93% red cells (RBCs), 6% platelets, 1% white blood cells (WBCs), and plasma. The goal of PRP is to maximize the number or concentration of platelets while minimizing the number of RBCs. Generally speaking, the higher the concentration of platelets, the better. Packed with growth and healing factors, platelets initiate repair and attract the critical assistance of stem cells. Because your own blood is used, there is no risk of a transmissible infection and a very low risk of allergic reaction.
How Often are Injections Given?
After the initial treatment, a follow up visit is scheduled 4-6 weeks later to check on healing progress. Some patients respond very well to just one treatment. However, typically 2-3 treatments are necessary. Injections are given every 4-8 weeks on average.
What Conditions Benefit From PRP?
• Rotator cuff injuries, including partial-thickness and full-thickness tears
• Shoulder pain and instability
• Tennis & golfer’s elbow
• Hamstring and hip strains
• Knee sprains and instability
• Patellofemoral syndrome and patellar tendinosis
• Ankle sprains
• Achilles tendinosis & plantar fasciitis
• Knee, hip, and other joint osteoarthritis
• Sports hernias & athletic pubalgia
• Other chronic tendon and ligament problems
In addition, PRP can be very helpful for many cases of osteoarthritis (the “wear & tear” kind).
• Knee arthritis
• Hip joint arthritis
• And other joint arthritis
Is PRP Covered by Insurance?
Most insurance plans, including Medicare, do NOT pay for PRP injections.
Do PRP Injections Hurt?
The level of discomfort of the treatment depends in part on the area being treated. For example, injections given into a joint often are minimally uncomfortable and in some cases painless. Injections given into tendons tend to be more uncomfortable. There is usually moderate pain for the next few days.
Anti-inflamatory medications (including Advil, Motrin, ibuprofen, Aleve, Celebrex, and Mobic) should be avoided five days prior to and 5 days after the injections,. These will interfere with the healing response. Tylenol is OK.
When Can I Expect to See Improvement?
On average, most patients start to see signs of improvement anywhere from 4-8 weeks after treatment. This can be less overall pain, an ability to do more activity before pain sets in, and/or faster recovery from pain. Because the goal of PRP therapy is to resolve pain through healing, lasting results are expected. Both ultrasound and MRI images have shown definitive tissue repair after PRP therapy, confirming the healing process. The need for surgery can also be greatly reduced by treating injured tissues before the damage progresses and the condition is irreversible
How long does it take?
The procedure takes approximately one to two hours, including preparation and recovery time. PRP is an in-office procedure which does not require general anesthesia, or hospital stays and without a prolonged recovery.
Are There Risks With PRP?
Anytime a needle is placed anywhere in the body, even getting blood drawn, there is a risk of infection, bleeding, and nerve damage. However, these are very rare. Other complications, though rare, can occur depending on the area being treated, and will be discussed by your doctor before starting treatment. Because PRP uses your own blood, you cannot be allergic to it.
Will PRP Help Me Avoid A Joint Replacement?
This is a frequently asked question. In the case of mild arthritis, PRP treatment may halt the development of further arthritic decay. However, in advanced arthritis, the goal of treatment is to reduce pain and improve function. In some cases the arthritis is so severe that PRP is not a viable option. In severe or advanced osteoarthritis PRP treatments may help delay the eventual need for a joint replacement, but it is rarely a treatment that eliminates the need for it. Some patients are not surgical candidates because of other medical conditions. Other patients simply do not want joint replacement surgery under any circumstance. In these cases PRP may be a viable treatment option, but it is not a permanent solution in these specific situations–treatments will need to be repeated periodically.
Additional Therapies
Fat Grafting
In the case of moderate to severe osteoarthritis and large tendon and muscle tears, such as rotator cuff, tennis elbow, and Achilles, simple PRP may be less effective because the liquid PRP has less tendency to stay in the tear; it leaks out. In order to combat this we often will combine PRP with fat to create a gel that fills the defect and promotes more effective healing. The fat is harvested from the patient’s belly, buttocks, or hips using a gentle liposuction technique. (The amount harvested generally is NOT enough to have a cosmetic effect.) The fat is concentrated via centrifuge, and the resulting fat concentrate is subsequently mixed with the PRP to create a gel. The gel fills the tear in the case of tendons/muscles, and helps maintain more constant contact with the joint surfaces in the case of arthritis.
Rehabilitation
To get maximum benefit from the treatment, and to help prevent re-injury, a specially-designed rehabilitation and exercise program is incorporated into your treatment. This helps the newly developing connective tissue mature into healthy and strong tendon or ligament fibers. In addition, nutritional support, such as glucosamine, MSM, and increased protein intake can help the healing process.
Stem Cell Injection Therapy
An exciting development in the treatment of chronic musculoskeletal conditions is the use of adult mesenchymal stem cells (MSCs).
What are Adult Mesenchymal Stem Cells?
Mesenchymal stem cells, or MSCs, are multipotent stem cells that can differentiate into a variety of cell types, including: osteoblasts (bone cells), chondrocytes (cartilage cells) and adipocytes (fat cells). MSCs are obtained from the bone marrow, most commonly the back of the iliac crest (the “hip bone”).
What Conditions Might Benefit From
Stem Cell Injections?
Stem cell injections are most commonly used for the treatment of conditions that have failed or responded incompletely to other more conservative treatments such as PRP and prolotherapy. Conditions include, but are not limited to:
• Osteoarthritis of the joints
• Chronic partial Rotator Cuff tears
• Persistent partial tendon tears, such as tennis elbow,
plantar fasciitis, quadriceps and patellar tendon tears.
• Partial muscle tears
• Meniscal (cartilage) tears in the knee
• Chondromalacia patella (patellofemoral syndrome)
Are There Risks Associated With Stem Cell Treatment?
Any injection is potentially at-risk for causing infection, bleeding or nerve damage. Risks will also vary depending on the structure(s) being injected. However, because we are using your own cells, you cannot be allergic. Also, because the injections are done under ultrasound guidance, the risks of damaging surrounding structures, or of injecting the wrong location, are almost completely eliminated.
How are MSCs Obtained?
Harvesting MSCs for injection therapy is done right in the office. The skin and the hip bone are numbed with lidocaine. A special needle is then passed through the cortex of the bone into the marrow cavity. This is a minimally painful procedure in most cases. The liquid marrow is then very slowly drawn into a syringe. Once an adequate amount of liquid marrow is obtained, the needle is removed and a bandage applied. The syringe containing the liquid marrow is placed in a special centrifuge. The marrow is spun and the stem cells are highly concentrated and passed into a new syringe from which the injection(s) are given. The entire procedure takes about an hour and is minimally uncomfortable.
Osteopathic Medicine
Osteopathy, or osteopathic medicine, is a system of health care based on viewing the patient as a whole, rather than as a collection of various parts. One of the distinguishing features of osteopathic medicine is the use of osteopathic manipulation (also known as osteopathic manipulative medicine (OMM) or osteopathic manipulative treatment (OMT)). Osteopathic physicians, or D.O.s, are fully licensed medical doctors, like M.D’s. They can specialize in all medical specialties, including family practice, cardiology, surgery, pediatrics, and so on. Osteopathic theory focuses on the body’s ability to heal itself. A.T. Still, M.D., the founder of osteopathy, claimed that the role of the physician was to “find health.” He viewed the body as a self-regulating, self-healing organism that only needed to be given an optimum environment in which to thrive. The goal of the osteopathic physician is to promote such an optimum environment. We refer to this as “Osteopathic Optimization”.
For more information go to www.osteopathic.org or www.academyofosteopathy.org.
Osteopathic Manipulative Medicine
Osteopathic manipulation is a medical procedure whereby the physician uses various types of manual or manipulative techniques to enhance the body’s self-healing capabilities. OMM encompasses the role of the bones, joints, muscles and ligaments, blood vessels, posture and biomechanics, and nerves in promoting health and treating disease.
The cornerstone of OMM is creating an ideal structure-function relationship in the body. If the body’s structure is optimized, then optimum function should follow. Before performing any osteopathic manipulative technique, the osteopathic physician takes an appropriate history and performs a physical exam to determine where problems may exist that could be interfering with the body’s self-healing ability.
Functional Health and Sport Medicine
352-512-0907 . www.fhmllc.net
Check Also
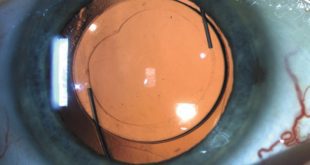
CUSTOMIZABLE LIGHT ADJUSTABLE LENS A GAMECHANGER FOR CATARACTS PATIENTS
All Americans have some degree of cataract change by the age of 75. As the …
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages