…AND EARLY DETECTION OF CERVICAL CANCER
 Each year millions of women make their annual trip to the gynecologist for their Pap test. Life continues as usual once they receive a postcard that is checked off as “normal.” But for many women, they receive a phone call from the doctor’s office indicating that their normal cervical cells have changed and now show precancerous cells or cancer. And this scenario is not uncommon. According to the American Cancer Society (ACS), in 2011, there were 12,710 new cases of invasive cervical cancer and 4,290 deaths in the United States. In its continued efforts to educate the community about the importance of early detection and prevention, InterCommunity Cancer Centers (ICCC)/Vantage Oncology (VO) in Lady Lake and Leesburg and InterCommunity Cancer Institute (ICCI) in Clermont are helping women increase their awareness about cervical cancer.
Each year millions of women make their annual trip to the gynecologist for their Pap test. Life continues as usual once they receive a postcard that is checked off as “normal.” But for many women, they receive a phone call from the doctor’s office indicating that their normal cervical cells have changed and now show precancerous cells or cancer. And this scenario is not uncommon. According to the American Cancer Society (ACS), in 2011, there were 12,710 new cases of invasive cervical cancer and 4,290 deaths in the United States. In its continued efforts to educate the community about the importance of early detection and prevention, InterCommunity Cancer Centers (ICCC)/Vantage Oncology (VO) in Lady Lake and Leesburg and InterCommunity Cancer Institute (ICCI) in Clermont are helping women increase their awareness about cervical cancer.
“Though deaths from cervical cancer have decreased over the past several years, this disease is still a great cause for concern,” said Bobby Harrison, M.D., radiation oncologist at ICCC/VO. “Detection and prevention are imperative to avoiding cervical cancer, and having a Pap test is thus far the most effective way to accomplish this.”
According to the ACS, normal cells in the cervix can gradually develop pre-cancerous changes that may turn into cancer. Some women with pre-cancerous changes of the cervix will develop cancer, but not all. The process may take several years, but it can also occur in less than one.
There are two important and clinically proven ways to stop cervical cancer from developing – preventing pre-cancers, and detecting and treating pre-cancers before they become cancerous.
Several critical risk factors are known to increase a woman’s chances of developing cervical cancer. They include, but are not limited to, the following:
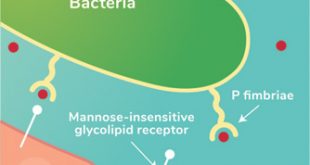
- Human Papillomavirus (HPV) Infection – Infection by HPV is considered the most important risk factor for cervical cancer. This disease is passed from one person to another through sexual (oral and intercourse) contact, as well as skin-to-skin contact with an HPV-affected area of the body.
- Smoking – Smoking can produce cancer-causing substances that are known to damage cervical cells’ DNA and may play a pivotal role in the development of cancer.
- Immunosuppression – Human immunodeficiency virus (HIV), the virus that causes AIDS, increases a woman’s risk for HPV infections. Women infected with HIV may develop a more invasive form of cancer because the virus severely weakens the body’s immune system.
- Family History – Women whose mother and/or sisters had cervical cancer are two to three times more likely to develop the disease themselves because they may possess the same genetic risk factors that make them more susceptible to infection.
Cervical cancer was once one of the most common causes of cancer death among American women, according to the ACS. But thanks to education and the increased use of the Pap test – a screening procedure that permits diagnosis of pre-invasive and early invasive cancer – the number of cervical cancer deaths in the U.S. continues to drop.
Women who have not had regular Pap tests represent the vast majority of clinically diagnosed invasive cervical cancers, reports the ACS. This procedure is used to obtain cells from the cervix for cervical cytology screenings. All women should have an annual Pap test about three years after they begin having vaginal intercourse, but no later than when they are 21 years old. Physicians strongly recommend that women continue cervical cancer screenings even after they have finished their childbearing years.
“By continuing to educate our patients about this potentially deadly disease we can significantly improve clinical outcomes and provide them a high quality of life,” said Maureen Holasek, M.D., radiation oncologist at ICCI.
For more information about cervical cancer, please visit the American Cancer Society at www.cancer.org/cancer/cervicalcancer.
THE EXPERIENCE OF INTERCOMMUNITY CANCER CENTERS
Having treated over 10,000 patients, ICCC and ICCI have 25 years of cancer-fighting experience. They are dedicated to empowering patients to have the confidence they need to change their lives. Radiation Oncologists Drs. Hal Jacobson, Herman Flink, Bobby Harrison and Maureen Holasek bring exceptional expertise in treating breast, lung, prostate, gynecologic, skin and other cancers.
As part of a larger, nation-wide oncology group of physicians and specialists under Vantage Oncology, the oncologists at ICCC and ICCI have access to aggregated clinical information and best practices from the treatment of more than 1,000 patients per day, enabling them to develop highly-effective and peer-collaborated treatments. This gives many of the centers that work with Vantage, including ICCC and ICCI, the ability to offer university-quality treatment services in smaller and more rural areas. It gives local communities exceptional services closer to home and in a non-hospital setting. To learn more, please visit ICCC at www.ICCCVantage.com and ICCI at www.careyoudeserve.com.
About Vantage Oncology
Vantage Oncology offers a complete development, implementation and management solution for radiation oncology practices. It provides ownership opportunities that empower physicians to maintain control of their practice while leveraging the strength of the company’s network and clinical resources. A multi-disciplinary team is committed to continuously raising the standards of cancer care. Vantage provides patients and their families with ultimate peace of mind through its commitment to clinical excellence and superior outcomes. For more information, please visit www.VantageOncology.com.
 Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages
Central Florida Health and Wellness Magazine Health and Wellness Articles of the Villages